Chronic pain is one of the most common conditions for which people seek medical attention, yet it is also one of the most misunderstood. The following article sheds light on pain management—a medical specialty known as physiatry—and dispels some of the myth and misinformation regarding the causes of and treatments for chronic pain.
Myth: Chronic pain is relatively uncommon and unlikely to affect me or someone I know.
Chronic pain is not uncommon. It affects an estimated 80 million Americans annually, and the impact is significant. According to the Yale Medical Group, chronic pain is the most costly health problem in the U.S., representing an aggregate expenditure of $62 billion annually in health care costs alone. That total rises to $100 billion when time off from work, lost wages and productivity are considered.
Myth: Most painful conditions are typically treated successfully.
It is estimated that 40 to 50 percent of pain patients fail to achieve adequate pain relief. Further, almost half of chronic pain suffers have changed doctors since their pain began and one in three patients has changed physicians three or more times due to a lack of relief or respect in regards to their pain complaints.
Myth: Pain is always a valuable reaction because it’s the body’s way of letting you know you have a serious problem.
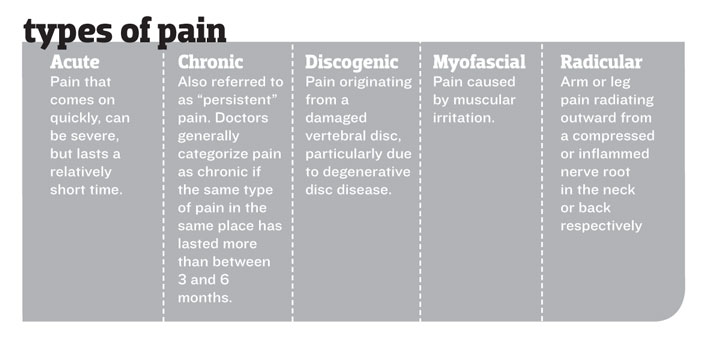
Acute pain typically indicates that the body has suffered a more serious injury or illness. Thus, pain can protect us from further injury by limiting activity or letting us know we need more immediate medical care. Chronic pain however, which is defined by pain lasting more than three to six months, is more likely due to a progressive overuse or degenerative condition, and as such serves no purpose beyond the suffering it causes.
Myth: Most pain conditions can only be treated effectively with surgery.
Interventional pain management is a recent and exciting medical specialty that offers options for patients who prefer to avoid surgery or for those who are not candidates for surgery. The advantage of this emerging field is that it offers less invasive treatment options and little to no recovery time.
Myth: Most pain management procedures need to be done at a hospital.
Today’s technologic advancements provide an expanding range of minimally invasive treatment options. Most if not all of these treatments are capable of being performed in an outpatient office setting with little to no downtime.
Myth: Pain is the inevitable result of aging.
While chronic pain does more commonly occur with age (often due to degenerative conditions such as joint arthritis or disc disease), no one should have to endure it. With proper treatment, pain can be managed effectively—no matter the person’s age.
Myth: I don’t need to see a doctor because most pain resolves itself.
It is true that most minor aches and pains from sprains or strains do resolve in short order. However, always get a diagnosis before dismissing a painful condition that could be something more serious. It’s critical to adequately address pain early on before it becomes chronic, which in many cases is a physiologic response of the nervous system “memorizing” and increasing the pain signal emanating from the spine—a process referred to as “wind-up.”
Myth: Most doctors have training in and are familiar with treating pain.
Not true. According to a recent joint statement issued by the Drug Enforcement Agency (which monitors the prescription writing of opiate pain medications) and 21 combined national health care organizations, the under-treatment of pain is a serious problem in the United States. This includes patients with chronic medical conditions and those who are critically ill or near death. Aggressive pain management is an integral and important aspect of quality medical care, because no patient should have to endure prolonged pain.
Myth: Since pain is so common, it is relatively easy to find a doctor who specializes in physiatry or pain management.
Despite the overwhelming scope of painful medical conditions, most patients in search of relief have difficulty finding access to providers who specialize in the discipline of pain management. In fact, the pain management field itself is in its infancy as it has only been recognized as a boarded specialty in the last decade.