In 2011, Jeopardy! champions Brad Rutter and Ken Jennings squared off in two exhibition matches against IBM’s Watson supercomputer. It may have been a test of man versus machine learning, but it was no contest. The human legends couldn’t keep up with Watson’s speed in response and accuracy at hitting Daily Doubles.
On the second day, a defeated Jennings wrote for his Final Jeopardy! answer, “I for one welcome our new computer overlords.”
That was eight years ago. Humanity witnessed a machine, a tool created by humans, challenge a cognitive ability that was thought to be uniquely human — the ability to win at Tuesday bar trivia. That, and the ability to process multiple intersections of data in working memory, eliminate false or unlikely responses, and find the most accurate solution faster and with a higher probability of success than human contestants who are considered the best at the same task.
Could we get that kind of big data in our continuum of health care?
Machine Learning is a Hot Topic
The excitement over artificial intelligence and medicine has been brewing since the golden age of science fiction. Recently, researchers discovered over 30,000 articles on machine learning and disease classification published in the past seven years, although only 69 had enough data to be useful for the researchers’ review.
“Many of the studies with terms like ‘artificial intelligence’ and ‘machine learning’ are just fad,” says Jacob McPadden, a post-doctoral fellow for the Yale Center for Medical Informatics. He’s working to use deep learning models to read sets of data (in one case, chest X-rays) on specific diseases. “Machine learning is the hot topic because it’s effective where some of the other traditional methods are not. But it also sounds cool.”
As of today no technology has been able to pass the Turing Test — a test of a machine’s ability to exhibit intelligent behavior equal to, or indistinguishable from, a human’s — and few have shown promise, even Watson. Instead, artificial intelligence, that is, machine learning, utilizes computer programs to match a patient’s data to a database and present a likelihood of an event based on that data.
With that in mind, the advancements in machine learning are promising in a wide range of medical services.
Improving Quality of Health Care
Because of machine learning’s ability to access a growing collective medical database, resources such as “predictive modeling and clinical decision support” will help reduce the chances of false positives in diagnoses.
As processing power and battery life increase, patients who are at a high risk of isolation during a medical emergency — like those who live alone — could be outfitted with monitors which send real-time data to doctors, including changes in vital statistics. If something happens, the monitor can send alerts to medical professionals and EMTs, even if the patient is unconscious. It’s the next generation of LifeCall.
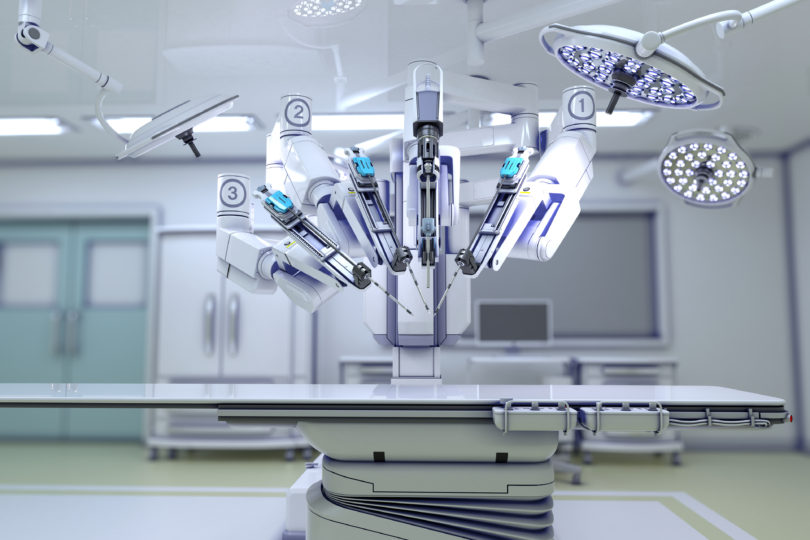
With big data, insurance companies can utilize artificial intelligence to provide consumers with more accurate risk assessments and faster service while reducing fraud. Surgery precision, prediction algorithms, incentives for healthy behavior and minimizing risk — these are just a few of the areas where machine learning can improve the quality of health care.
Earlier this year, Virginia-based Optima Health, the health insurance subsidiary for Sentara Healthcare, announced it was partnering with Cardinal Analytx Solutions, an AI-enabled health insights company in Palo Alto, Calif. The software’s predictive capabilities allow Optima to identify patients who are at a rising risk of health decline.
For example, the computer looks at a patient’s health patterns — say someone is a smoker — and makes a determination as to whether he could benefit from early outreach and intervention. It allows Optima’s care management team to then reach out and offer help, such as a smoking cessation program.
The raw data comes from historical information such as plan enrollment and claims. The computer ingests that data and identifies at-risk people. “Every time we run this, it relearns,” says John Coughlin, vice president of informatics and analytics at Optima. The constant improvement “makes the information we pass on all that more helpful,” he adds.
Still, Questions Remain
However, there are legitimate questions from patients and doctors. While legislation such as the Health Insurance Portability and Accountability Act (HIPAA) provides guidance in patient information management, including what information can and cannot be sent to third parties, the fact that this personal information exists in the first place gives some consumers pause.
Privacy is also an issue. Once that information is released, there is no way to remove it. Coughlin assured that at Optima, the information is not “going to be used against” patients, such as to raise premiums.
“Our focus is on our members’ health, helping them live healthier lives,” Coughlin says.
The medical education world is struggling to keep up as well. In his recent article, “The Empirical Challenge of 21st Century Medical Education,” Steven Wartman argues for an immediate overhaul of the curriculum and teaching strategies of the medical classroom. He would know — he’s the president of the Association of Academic Health Centers (AAHC), a non-profit which seeks to improve health care through the advancement of medical education.
Wartman emphasizes the need for reforms in the curriculum because the human-machine dynamic duo is coming, and doctors better be ready to play their part. While computers can gather data faster, it is imperative that doctors “learn to find and understand information that is trusted and accurate,” he says.
The Evolving Medical Field
But as important as teaching students how to work with machines, Wartman says, “[t]he cultivation and mastery of empathy and compassion … must be the foundation of the profession.” The medical field must evolve with technology if it hopes to achieve the continuing goal — to provide the best possible treatment for each patient in need.
“Data management and communication between institutions will make these machine learning ideas functional,” McPadden says. “We can do amazing things with it, but the argument that machine learning is going to take the place of human physicians is a bizarre idea. It’s a tool. It can only learn simplistic questions — you have to know the right questions to ask and what the answer is going to look like.”
McPadden says we need to keep in mind that the algorithms are only as good as the dataset we give these machines. “A majority of studies are limited in that they are not yet scalable, and we also don’t know exactly what these algorithms are really learning. You don’t want [technology] failing in the odd times, you want it to be its best — physician expertise can recognize stuff that an algorithm can’t be taught … yet.”
There are a few things still innately human — to listen to patients, to feel compassion for them, to empathize with them — to do what so many doctors have said is the best part of the profession. For now, artificial intelligence has a long way to go before its widespread usage in medical offices to support, not supplant, the physician.