TPMG surgeon plans to offer customizable hernia repair with newly acquired robotic surgery technology.
Over the last decade, robot-assisted surgery has steadily become a fixture in operating rooms across the country and continues to gain in popularity with surgeons as a minimally invasive surgical technique.
This fall, Dr. Steven Hopson, a general surgeon and hernia specialist at TPMG General Surgery and Hernia Center in Newport News, Va., will be among a handful of surgeons in the Hampton Roads area to offer an innovative technology for hernia repair.
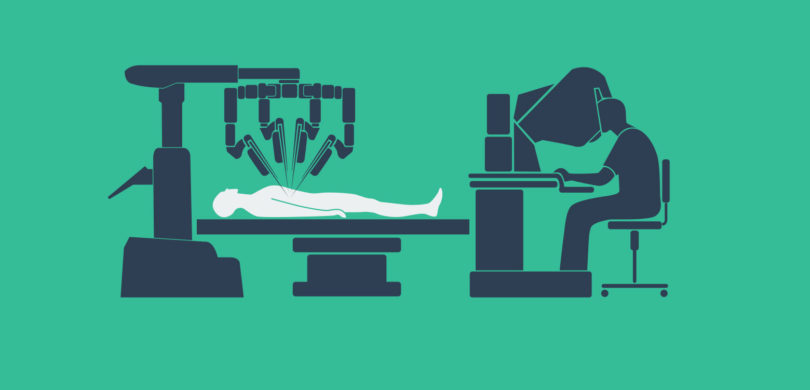
Using robot-assisted surgery, or RAS, Hopson will be able to perform procedures with more ease, efficiency and precision than ever before — all while controlling the instruments from a nearby console.
“Having this technology as part of my practice allows me to provide options suited to the specific needs of each surgical case and patient,” Hopson says.
Surgical Hernia Treatment
“A hernia occurs when an organ or tissue pushes through an opening or weak area of the abdominal wall, upper thigh or groin area either due to a preexisting weakness at birth or strain,” Hopson says.
Depending on the area, a hernia may resolve on its own. However, if it doesn’t, surgery is often the only treatment to avoid serious, life-threatening complications. Factors including the hernia type, medical history, lifestyle, availability of post-operative care at home and recovery are all considered to determine the appropriate surgical approach for each case.
Historically, hernia repairs have been successfully completed using open repair and laparoscopic approaches.
Depending on the specific case, in an open repair a large incision is made to view the protrusion and reinsert the tissue or organ to its original area. The opening is then closed with sutures and may be secured with mesh to strengthen the area and prevent further occurrences.
With the laparoscopic approach, small incisions are made at the insertion point for the instruments to complete the repair — one of which is an endoscope, a long tube-like instrument with a camera that allows the surgeon to view the operation. Patients who undergo this minimally invasive approach typically experience less pain and a quicker recovery time.
With robotic surgery, the surgeon is effectively performing the same procedure as with an open or laparoscopic approach. But because the instruments articulate and mimic the surgeon’s movements in a way that is limited in the laparoscopic approach, the surgeon is able to operate with more ease, efficiency and precision.
The instruments are positioned through small incisions similar to the laparoscopic technique, but rather than the physician directly handling the instruments at the operating table, the physician sits at a nearby console to view the operation and control the instruments.
Determining the Right Approach
While robotic surgery may offer multiple benefits such as quicker recovery, less pain and smaller, less-noticeable scars, it is important to note that traditional open and laparoscopic techniques remain sound surgical options for hernia repair, Hopson says.
“My goal is always to offer patients options and state-of-the-art care, but I do utilize the open and laparoscopic approaches in my practice … the needs of each specific case are always paramount when determining the surgical technique,” he says.
Some patients, due to a variety of factors, may not be candidates for RAS. For instance, a patient with a complex hernia repair may benefit from an open surgery, while a patient with a straightforward hernia repair may be better suited to a laparoscopic approach.
As robotic surgery is still relatively new to the general surgery field, it could still be a while before the technology is considered the gold standard in hernia repair.
“While there is evidence of success with robotic surgery, the technology is still unproven as a superior approach to treatment over other methods used for general surgery,” Hopson says. “We still have a ways to go before robotic surgery is commonplace in our field.”